Root Canal Treatment
Root Canal Treatment
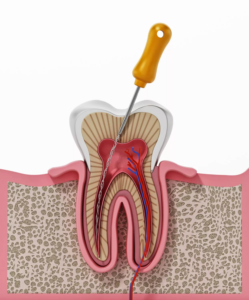
Root canal treatment, also known as endodontic therapy, is a dental procedure to save a tooth that is badly damaged or infected. The procedure involves removing the soft tissue inside the tooth, called the pulp, which contains nerves, blood vessels, and connective tissue.
Here’s a breakdown of root canal treatment:
Why is a Root Canal Needed?
A root canal becomes necessary when the pulp inside a tooth becomes inflamed or infected due to:
- Deep decay: Bacteria can reach the pulp.
- Cracked or chipped tooth: Bacteria can enter the pulp through the damage.
- Repeated dental procedures on a tooth.
- A faulty crown or filling.
- Trauma to the tooth: Even if the tooth isn’t visibly cracked.
Signs You Might Need a Root Canal:
- Severe toothache, especially when chewing or applying pressure.
- Prolonged sensitivity to hot or cold temperatures, even after the sensation is removed.
- Darkening of the gums or tooth.
- Swelling and tenderness in the gums.
- A persistent or recurring pimple (boil) on the gums.
- A chipped or cracked tooth.
The Root Canal Procedure:
Root canal treatment typically involves the following steps and can usually be completed in one or more appointments:
1. Diagnosis and X-ray: The dentist will examine the tooth and take X-rays to determine the extent of the damage and the shape of the root canals.
2. Anesthesia: Local anesthesia is administered to numb the tooth and surrounding gum tissue, so you should feel little to no pain during the procedure. If you have dental anxiety, your dentist may offer sedation options
3. Dental Dam: A thin sheet of rubber called a dental dam is placed over the tooth to isolate it and keep it clean and free of saliva during the treatment.
4. Access Hole: The dentist creates an opening in the crown (top surface) of the tooth to reach the pulp chamber and root canals
5. Cleaning and Shaping: Using small dental instruments called files, the dentist carefully removes the infected or damaged pulp tissue from the root canals. The canals are then cleaned, disinfected with antiseptic solutions, and shaped to prepare them for filling. This step is crucial to eliminate bacteria and infection
6. Filling the Canals: Once the canals are thoroughly cleaned and shaped, they are filled with a biocompatible material, usually a rubber-like material called gutta-percha, along with an adhesive cement to ensure complete sealing. This prevents bacteria from re-entering the tooth
7. Temporary Filling: A temporary filling is usually placed to close the access hole and protect the tooth until the permanent restoration
8. Crown Placement: In most cases, a permanent crown is necessary to protect the treated tooth and restore its function and appearance. A crown is a custom-made cap that covers the entire tooth. The dentist will take impressions of your tooth to create the crown, which is typically placed at a subsequent appointment. In some cases, if the tooth is not significantly weakened, a permanent filling might be sufficient.
Success Rate:
Root canal treatment is generally a highly successful procedure, with success rates ranging from 86% to 98%. The long-term success of a root canal depends on factors such as:
- Proper cleaning and sealing of the root canals.
- The tooth receiving a final restoration (usually a crown) in a timely manner.
- Maintaining good oral hygiene.
- Regular dental check-ups.
Aftercare:
Following a root canal, it’s important to:
- Avoid chewing on the treated side until the permanent restoration is in place.
- Take any prescribed pain medication as directed. Over-the-counter pain relievers like ibuprofen or acetaminophen are often sufficient.
- Maintain good oral hygiene by brushing and flossing regularly.
- Schedule and attend your follow-up appointment for the permanent crown or filling.
- Contact your dentist immediately if you experience severe pain, swelling, or any other concerning symptoms.
Book your Appointment Today!
Your smile is just one click away.
